Researchers Help People Lead Healthier Lives at Home

09/01/2024
By Ed Brennen
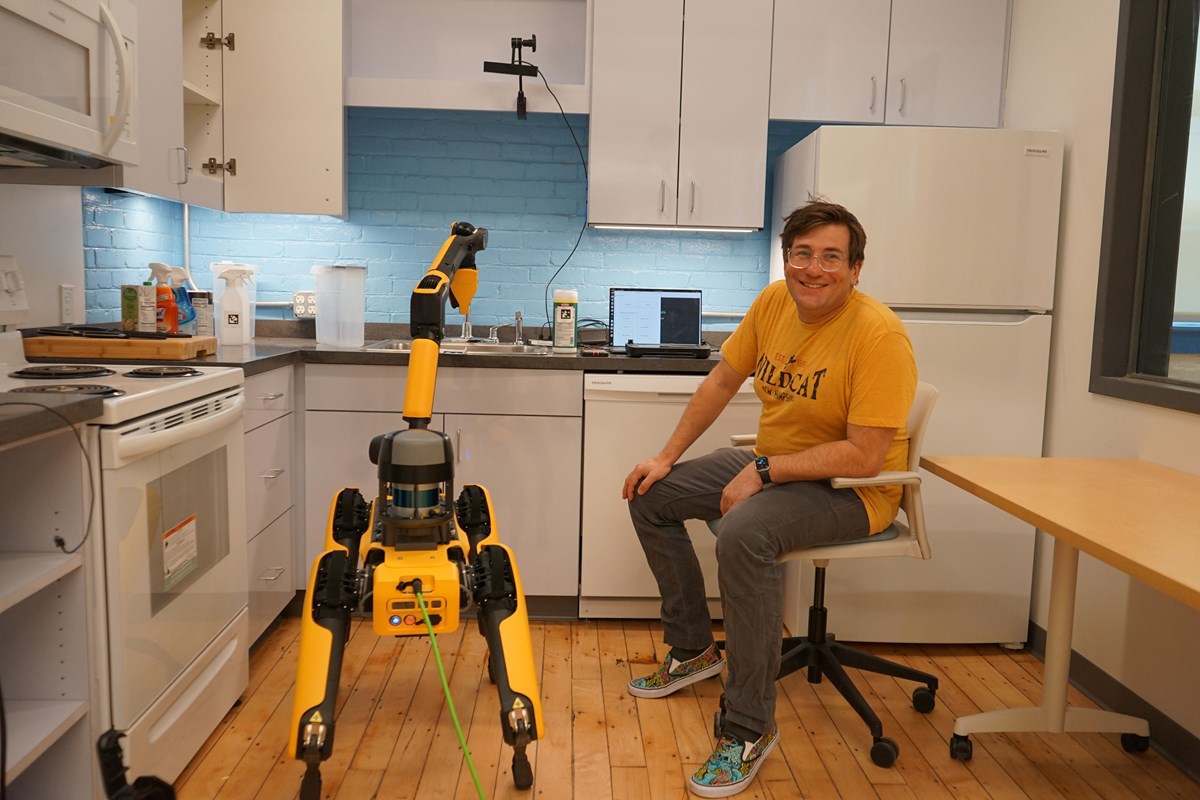
Electrical engineering Ph.D. student Russell Perkins ’18, ’20 is sitting in a kitchen, patiently training a dog. It is no ordinary dog, however, and Perkins is not teaching it typical moves like “sit” and “heel.”
Rather, Perkins is working with Spot, a $75,000 robot dog made by Boston Dynamics. In a simulated kitchen in the Lowell Advanced Robotics Initiative (LARI) Laboratory at Southwick Hall on North Campus, he is showing Spot how to pick up cleaning products from a countertop.
“He’s a good boy,” Perkins says as Spot uses the gripper at the end of its arm-like head to carefully clamp a container of cleaning wipes—movements that are tracked by cameras mounted on the kitchen cabinets and displayed on Perkins’ laptop.
The training session is part of AI-CARING, or the AI Institute for Collaborative Assistance and Responsive Intervention for Networked Groups. Supported by a $20 million grant from the National Science Foundation, the project is developing artificial intelligence systems that improve the quality of life and independence of aging adults living at home.
Paul Robinette, an assistant professor in the Department of Electrical and Computer Engineering, is co-principal investigator on the project. It is led by Computer Science Prof. Holly Yanco in collaboration with seven other universities, including Stanford, Carnegie Mellon and Georgia Tech.
AI-CARING is just one of the ways in which faculty researchers from the Francis College of Engineering are developing medical technologies, apps and devices to diagnose, treat and care for older adults and people with disabilities.
In the Department of Biomedical Engineering, Prof. Emeritus Bryan Buchholz is co-PI on CAPCaT, or the Center for Advancing Point of Care Technologies. Launched in 2018 as an offshoot of the Massachusetts Medical Device Development Center (M2D2), a collaboration between UMass Lowell and UMass Chan Medical School, CAPCaT is helping startup companies and entrepreneurs to develop medical devices that can be used at home by patients with blood, heart, lung and sleep conditions. It is supported by the National Institutes of Health (NIH), which followed an initial five-year, $7.9 million grant with a five-year, $8.9 million award in 2023.
“Some of these projects are going to help people that are not getting help right now, which is the most satisfying thing about the work,” says Buchholz, who is co-PI with David McManus, chair of the Department of Medicine at UMass Chan, and Nathaniel Hafer, director of M2D2.
CAPCaT is feeding a growing consumer demand: The global home diagnostics market generates $5 billion annually and is expected to nearly double by 2032, according to the market research firm Precedence Research. One reason for the boom is the COVID-19 pandemic, when, out of necessity, clinicians and patients embraced the convenience and reliability of at-home devices (also known as point-of-care technologies).

“Point-of-care devices are a lot more acceptable now than they were prior to COVID,” Buchholz says.
Over its first six years, CAPCaT has awarded $3.4 million to 27 projects, which have gone on to secure $47 million in post-award funding.
“We are a pass-through organization,” Buchholz explains. “We get the money from NIH and then have a competition where people apply for funding. We have a stringent review process and select the best ones and pass that money on to those companies.”
One early success story is Sanguina, a point-of-care test for anemia that received nearly $94,000 in CAPCaT funding in 2019; it earned Food and Drug Administration approval last year and is now available over the counter. Another is Wellinks, a digital health care company that provides a first-of-its-kind virtual platform for at-home management of chronic obstructive pulmonary disease (COPD). It received $105,000 in CAPCaT funding last year, and is now being used by a growing number of health care institutions.
The Lift Program
Buchholz is also the PI on another M2D2 offshoot, the UMass Lowell Innovative Fellows Training (LIFT) program. Backed by a five-year, $1.2 million grant from the National Institute on Aging, LIFT offers experiential biotech and med-tech learning opportunities for graduate students and postdoctoral researchers working in the fields of aging and aging-related diseases, including Alzheimer’s.
“The idea is to train doctoral students in careers other than academia by teaching them about innovation and entrepreneurship,” says Buchholz, whose co-PIs are Asst. Prof. Yanfen Li of Biomedical Engineering and Assoc. Prof. Denise Dunlap of Marketing, Entrepreneurship and Innovation.
LIFT’s inaugural 2024 cohort of 10 fellows included Perkins, the UML electrical engineering Ph.D. student who works with Spot, the robot dog. Over the course of the 14-week LIFT program, Perkins developed SafeGuardian AI, an artificial intelligence-driven, in-home robot that can alert people to potential scams by monitoring their emails and phone calls.
“In addition to the financial loss, there’s a profound emotional impact on victims,” says Perkins, who was inspired to create the device after a relative was scammed out of $1.6 million.
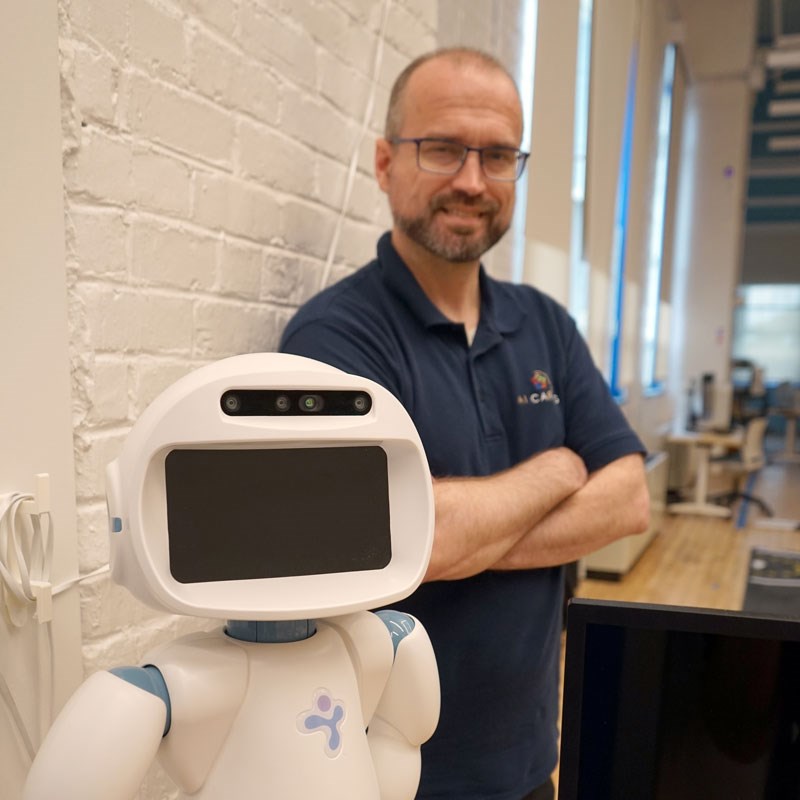
Having a robot in the home, be it a four-legged Spot or a stationary device like the QTrobot (which can also be found in the LARI Lab), requires an element of trust from the user. That is the focus of Robinette’s research work for AI-CARING.
“If you don’t trust a system, you’re not going to use it,” says Robinette, who joined UML in 2019 from MIT. “People don’t necessarily know what a system is capable of or how to work with it. Bridging that gap is hard, and one of the problems is trust.”
Collecting personal data creates one of the biggest trust issues. An AI system can help an older adult to live in their home longer by monitoring their health with cameras, microphones and other sensors, but how do they know for sure who has access to their data?
“We can give people the ability to control that, but that means they have to trust that the system is actually going to keep their information,” Robinette says.
“I’m looking at my grandparents and even my parents and thinking about what they’re going to need in the coming years, and how we can best accomplish that.” -Asst. Prof. Paul Robinette
Another type of trust involves calibration. A person can demonstrate to Spot how to load their dishwasher—silverware in the basket, cups and bowls on the top rack—but it could make a mistake. It could place the bowls face-up, for instance.
“Is the person going to say, ‘Oh, the robot’s broken. It doesn’t work,’ or are they going to give it another chance? Because all it needs is more information,” Robinette says.
The AI-CARING team is exploring whether an AI system can be considered more trustworthy simply by saying “sorry.” If a person asks their AI bot a question and it takes too long to answer, the person may not trust the answer as much, Robinette says.
Using ChatGPT, the team wants to use the person’s verbal feedback to produce an apology specific to the complaint. “It could say, ‘I’m sorry I took too long to answer your question. I’ll think about it more next time,’” Robinette says. “It’s another step in bridging that gap.”
According to a 2021 survey by the American Association of Retired Persons, 77% of adults over the age of 50 prefer to age in place. Robinette says it is “definitely rewarding” to know that AI-CARING is helping people do just that.
“I’m looking at my grandparents and even my parents and thinking about what they’re going to need in the coming years, and how we can best accomplish that,” he says. “There certainly aren’t enough people in caregiving institutions, so if we can supplement that with robots, everything will be a little easier."
