September 2022
Using Participatory Ergonomics to Address Patient Handling Injuries in a Community Hospital (pdf)
Contributed by Alicia Kurowski, Sc.D., Research Professor, Department of Biomedical Engineering, UMass Lowell
The health care industry employs more than 18 million workers in the US, and patient care-related injuries, especially those related to moving patients, are a common cause of work disability in this industry. Manually lifting, transferring, and repositioning patients have resulted in high rates of disabling back injuries and other musculoskeletal disorders (MSDs) in hospitals, nursing homes, and other health care settings. Ergonomic interventions to minimize exposure to manually moving patients by use of slings, mechanical lifts, and patient transfer aids have become the primary strategy to prevent these problems, and have been shown to lead to significant reductions in number of injuries, workers’ compensation claims, and related costs.1
In partnership with Frisbie Memorial Hospital in Rochester, New Hampshire, the Healthy Workplace Participatory Program (HWPP) was employed in early 2014. It is designed specifically to help employer organizations adopt and implement programs with a Total Worker Health® approach. The HWPP was developed to engage employees in designing integrated solutions that address a wide range of work environment, work organization, safety, and employee health issues.
Using the HWPP, a participatory ergonomics-based method was used to develop interventions that mitigate root causes underlying patient handling injuries. The question was, why were these injuries happening? To investigate, the HWPP was implemented in a high incident location on a medical/surgical unit at Frisbee. The hospital’s ergonomics team was comprised of front-line workers and led by a program Champion. They addressed patient handling injuries using the Intervention Design and Analysis Scorecard (IDEAS) Tool, a research-based, intervention design tool used in the HWPP.2
Recent injury data alone did not provide complete information to understand root causes for patient handling injuries so the ergonomics team used the IDEAS tool, recruited more direct patient care staff to participate, and surveyed patient care staff on the unit. The team identified equipment, staffing/irregular breaks, and lack of exercise/inadequate sleep as root causes of patient handling injuries. Frisbee staff, trained by researchers in these tools, developed interventions to address each root cause for injuries and determined solutions to address them. The team presented their three interventions, with business case analyses, to hospital leaders for approval and funding. Leadership approved an equipment-oriented intervention that included purchasing ceiling lifts; implementing systems for sling coding, storage, and laundering; providing enhanced equipment and super-user training; and updating core competencies.
In the two-year period from pre- to post-intervention, rates of patient handling injuries per 100 full-time employees decreased by 44% hospital-wide. Over the next five years of follow-up, direct costs of patient handling injuries continued to remain far lower than pre-intervention injury costs. In some years the number of injuries increased; however, costs were low, indicating reduced injury severity.
The HWPP Toolkit facilitated engagement of caregiving staff in the design of interventions that were successful for reducing injuries and associated costs. Contextual factors contributing to success were active employee engagement, the presence of an enthusiastic program advocate (Champion), and the hospital’s continuous improvement culture. Several intervention components were disseminated hospital-wide. Intervention evaluation continued to show cost savings and injury reduction five years after initiating the program.
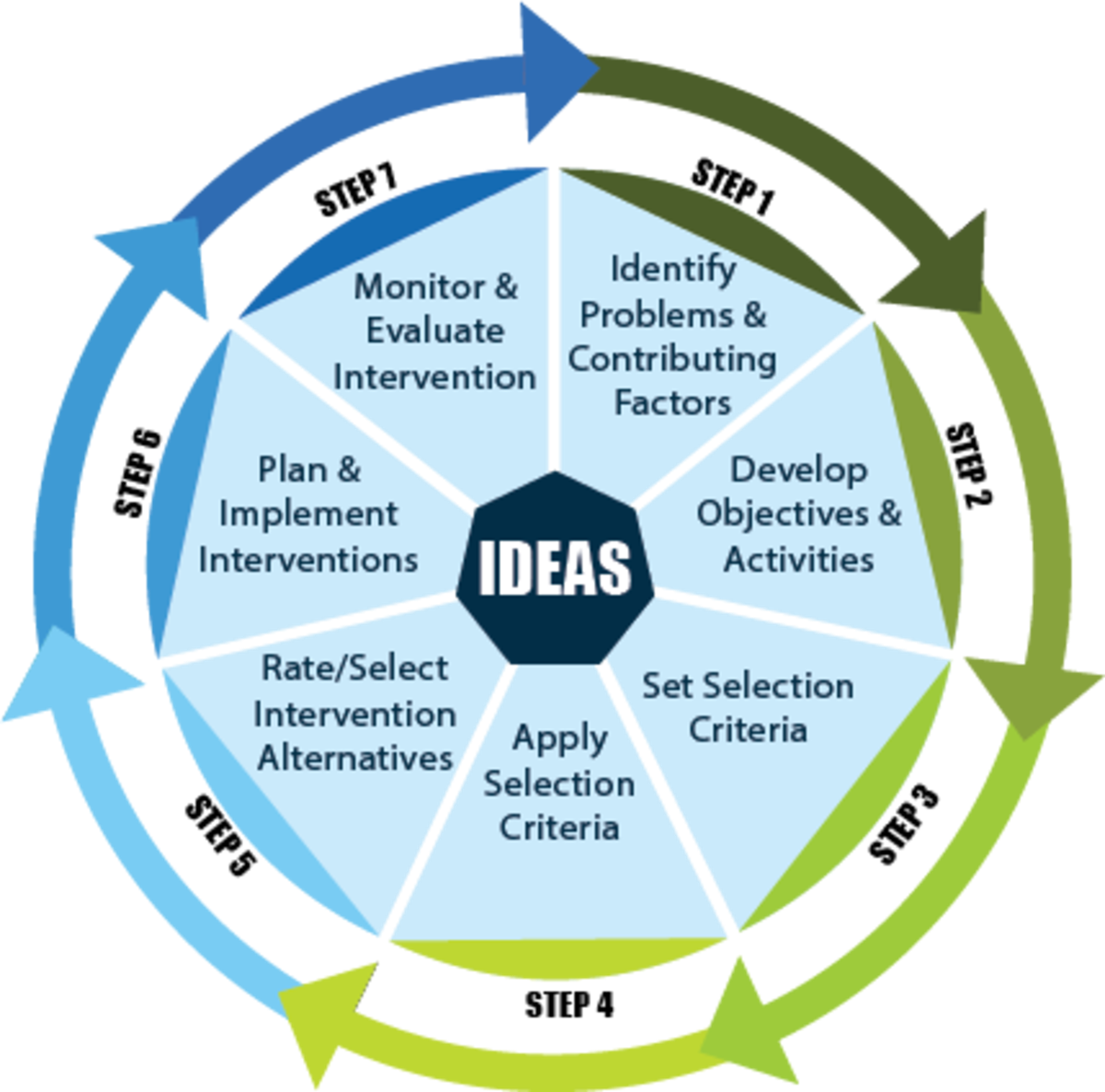
Diagram 1: IDEAS Tool
References
- Kurowski, A., Pransky, G. & Punnett, L. Impact of a Safe Resident Handling Program in Nursing Homes on Return-to-Work and Re-injury Outcomes Following Work Injury. J Occup Rehabil 29, 286–294 (2019). https://doi.org/10.1007/s10926-018-9785-7
- Robertson, M., Henning, R., Warren, N., Nobrega, S., Dove-Steinkamp, M., Tibirica, L., Bizarro, A., & CPH-NEW Research Team (2013). The Intervention Design and Analysis Scorecard: a planning tool for participatory design of integrated health and safety interventions in the workplace. Journal of occupational and environmental medicine, 55(12 Suppl), S86–S88. https://doi.org/10.1097/JOM.0000000000000036
Alicia Kurowski, Sc.D., is a CPH-NEW funded researcher, the Principal Investigator for Embedding Employee Participation in Safety and Health through Integrated Facilitated Teams (SHIFT II). This multi-phase participatory research study addresses the health, safety, and wellbeing of health care workers with the objective to evaluate new strategies for embedding employee participation into health & safety infrastructure (in a healthcare facility & through union-based training).
CPH-NEW is a NIOSH Center of Excellence for Total Worker Health®. CPH-News & Views is a quarterly blog written by center researchers and guest authors on emerging topics related to healthy workplaces. We welcome your responses and discussions. Please send all comments to CPHNEW@uml.edu.
Total Worker Health® is a registered trademark of the U.S. Department of Health and Human Services (HHS). Participation by CPH-NEW does not imply endorsement by HHS, the Centers for Disease Control and Prevention, or the National Institute for Occupational Safety and Health (NIOSH). This publication was supported by NIOSH Grant Number 1 U19 OH012299. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH or CPH-NEW.
